Physiotherapy: A Path to Rehabilitation for Frozen Shoulder
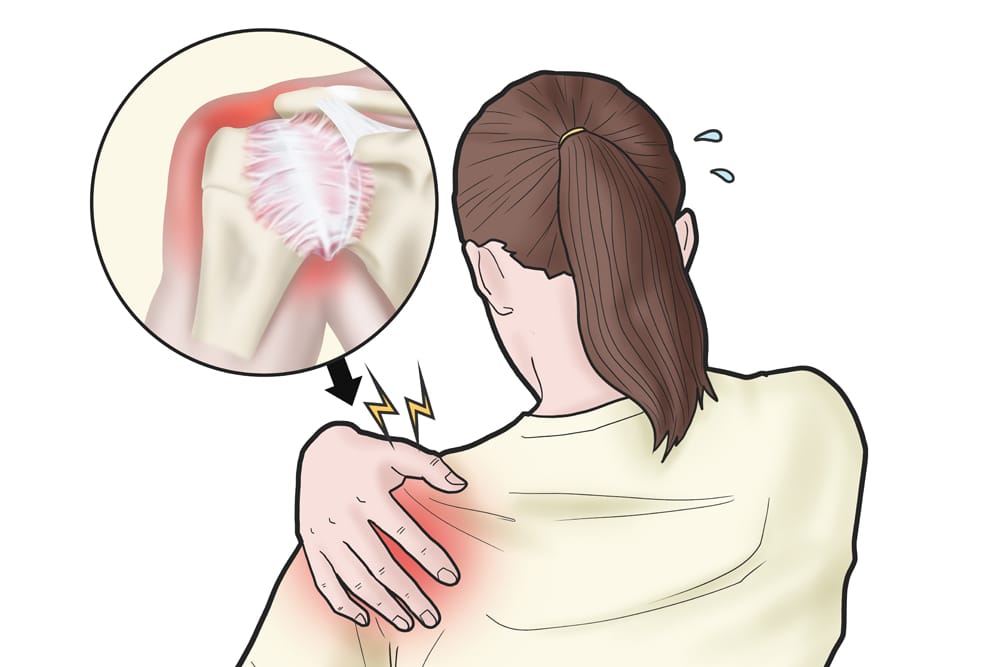
Frozen shoulder, also known as adhesive capsulitis, is a condition characterized by stiffness and pain in the shoulder joint. It typically develops gradually, gets worse over time, and then resolves, often taking one to three years to reach its course. This condition can significantly impact an individual’s daily activities and quality of life, making even […]
Medial and Lateral Ankle Sprain Physiotherapy: A Comprehensive Guide

Just one wrong step can unexpectedly lead to an ankle sprain. Ankle sprains are among the most common injuries encountered, especially in athletes and physically active individuals, according to this resource. Understanding the differences in treatment between medial and lateral ankle sprains is crucial for effective recovery and prevention of future injuries. This guide will […]
Understanding and Managing Chronic Pain with Physiotherapy

Chronic pain, a complex and often debilitating condition, affects millions of people worldwide. Per Physiopedia, Chronic pain is a leading source of human suffering and disability. Unlike acute pain, which is a natural response to injury and typically resolves once the injury heals, chronic pain persists long after the injury has healed, sometimes even without […]
Shin Splints & Physiotherapy: A Comprehensive Guide to Treatment and Prevention

The term “shin splints” is often viewed as a broad and inclusive phrase that encompasses various leg-related conditions. Shin splints, medically known as “idiopathic compartment syndrome” or “medial tibial stress syndrome,” are a common condition that affects athletes, runners, and even the average person who has suddenly increased their level of physical activity. The pain […]

